News
Western Queensland Primary Healthcare AOD Capacity Development
From May 2021 to December 2022 QNADA embarked on a project supported by WQPHN and QNADA to facilitate AOD capacity development within primary healthcare services in Western Queensland. It goes without saying, Western Queensland is vast and sparsely populated, meaning there are unique challenges to health service access and delivery across this region. Western Queensland has a predominantly generalist health workforce and a limited availability of alcohol and other drugs (AOD) specialist services[1].
Primary healthcare services in the region have the potential to serve as an initial point of contact for people who use alcohol and other drugs and for those who have concerns with their use, by playing a critical role in facilitating appropriate care and follow up, particularly at an early stage[2],[3],[4]. The role of primary healthcare services can include informal conversations about a person’s relationship with substances through to formalised AOD screening and brief intervention, supporting referrals to specialist AOD services, and contributing to enhanced continuity of care[5],[6]. However, primary healthcare services often report a lack of confidence and skills to provide adequate AOD care, which is compounded by barriers such as stigma and discrimination and workforce shortage[7],[8].
QNADA, in partnership with external stakeholders, delivered and facilitated a range of activities throughout the project, including:
- providing individual primary healthcare practice support
- establishing regional service level network meetings
- coordinating the delivery of ASSIST (Alcohol, Smoking and Substance Involvement Screening Test) training
- reviewing alcohol and other drugs related HealthPathways
- delivering an AOD in primary healthcare toolbox talk
- drafting an easy to use information resource for primary healthcare practitioners responding to AOD issues
- promoting existing resources (eg Adis 24/7, ADCAS, Insight).
The project had a small number of participants however key findings from the project evaluation indicated an overall positive impact. For example, an increased level of confidence was found in using alcohol and other drug specific screening and assessment tools (e.g. ASSIST), delivering brief intervention to patients, and matching referrals to patient needs. An increased level of knowledge was also found in some key alcohol and other drug concepts (eg harmful drug use, alcohol and other drug dependence), and in alcohol and other drug information services (eg HealthPathways, Alcohol and Drug Clinical Advisory Service). In addition, several enablers for primary healthcare services to deliver good practice AOD responses in Western Queensland were identified. At the service level, these included having accurate and informed knowledge around patterns of alcohol and other drug use, the range of AOD treatment types, and local referral options, and maintaining collaborative relationships between key workers among services. At the system level, having face to face engagement and networking opportunities (eg network meetings) for workers, and a stable and engaged workforce (eg consistent staffing within a practice) is also likely to contribute to better provision of alcohol and other drug care.
However, at a systems level, the lack of alcohol and other drug specific MBS item numbers, high workforce turnover, and excessive distance between services all contribute to challenges for primary healthcare services in providing AOD support. These issues will continue to inform QNADA’s advocacy into the future as part of our ongoing work with other state and territory partners and the national AOD peak, Australian Alcohol and other Drug Council (AADC).
In the short to medium term, there are opportunities to address a range of barriers identified in the evaluation including:
- further strengthening linkages between primary healthcare services and their locally available specialist alcohol and other drug treatment services
- continuing to address stigma that is associated with illicit drug use and negative connotations around seeking alcohol and other drug treatment, which created challenges for both providing and seeking support
- addressing concerns around lack of anonymity in small towns in order to increase help seeking
- responding to specific concerns around the normalisation of high quantity and frequency alcohol use.
In future QNADA hopes to continue our activities supporting primary healthcare services in the Western Queensland region by:
- continuing to facilitate local workforce linkage across the Western Queensland region through AOD focused service level networks.
- continuing individual practice engagement to enhance alcohol and other drug responses in primary healthcare services.
- facilitating and supporting ongoing alcohol and other drug related professional development and upskilling opportunities for primary healthcare services, with a focus on staff most likely to provide an AOD response (eg practice nurses).
While QNADA is pleased with the progress we’ve made in this space, this represents a first step to enhancing AOD responses in primary healthcare settings. We’d like to thank WQPHN for their support in funding this project and all the service providers and project partners who participated. Thank you!
————————————————–
[1] Western Queensland Primary Health Network, “A Five-Year Plan (2021-2026) to Improve Mental Health, Suicide Prevention and Alcohol and Other Drug Treatment Services in Western Queensland,” (2021).
[2] Queensland Mental Health Commission, “Achieving Balance 2022-2027: The Queensland Alcohol and Other Drugs Plan,” (2022).
[3] Queensland Health, “Better Care Together: A Plan for Queensland’s State-Funded Mental Health, Alcohol and Other Drug Services to 2027,” (2022).
[4] Michala Kowalski and Liz Barrett, “Engaging General Practice and General Practitioners in Alcohol and Other Drug Treatment,” in Drug Policy Modelling Program Monograph (University of New South Wales, 2020).
[5] Ibid.
[6] Queensland Health, “Better Care Together: A Plan for Queensland’s State-Funded Mental Health, Alcohol and Other Drug Services to 2027.”
[7] Western Queensland Primary Health Network, “A Five-Year Plan (2021-2026) to Improve Mental Health, Suicide Prevention and Alcohol and Other Drug Treatment Services in Western Queensland.”
[8] Kowalski and Barrett, “Engaging General Practice and General Practitioners in Alcohol and Other Drug Treatment.”
Data linkage across systems
Maria Ortiz
There is limited use of data to understand the engagement of people who use drugs (PWUD) in other systems such as the Child Safety, Criminal Justice and Youth Justice systems. Capturing and reporting of data is a critical part of informing and supporting better policy decisions by identifying the needs of PWUD and their families and friends in Queensland. We need this information to build an understanding of the effect that multiple contacts with different systems have on people with complex needs.
Data is also key to support a continuous improvement approach to Alcohol and other Drugs (AOD) treatment service delivery. Improved data collection would strengthen the development of policies to reduce harm and improve the ability to report on the prevalence of AOD treatment services across different systems in Queensland. With the support and perspective from multiple agencies, this would lead to better capturing of the frequency in which people with complex needs are involved in different systems.
The use of existing data (such as the National Drug Household Survey, AOD Treatment Services NMDS or the National Alcohol Indicators Project – the most prominent sources for drug-related data) is a cost effective way of identifying patterns of substance consumption and treatment within a community, and a reliable way to assess trends over time.[1] However, there are some limitations with the use of datasets that are not designed to answer the question of interest, and caution shall be taken when making conclusions to avoid misleading findings. Substantial amounts of data are collected throughout all systems, but it is gathered in ways that constrain the potential information we can obtain from it. Therefore, even though the system is data rich, it is also information poor.
Why is it important that we address data gaps?
Data quality is a measure based on validity, completeness, accuracy, and how current the data is. Advocates give data-based arguments to policy-makers in reports or inquiries, this is significant as the policy implementation approaches often draw upon the findings of these reports. The growing demand for transparent, accountable and responsive reporting from our governments is progressing the availability and volume of data. This is why it is important we address current data issues.
All information comes from raw data that without being organised can be challenging to understand. Drawing insights from raw data involves losing a certain amount of data to facilitate its interpretation. This is when there is greater risk to make misleading or invalid statements. Often these statements are somewhat correct but don’t give the full context.
Inaccurate data needs to be identified to ensure that decision-makers and other users are working with accurate information. Improved data collection/reporting methodologies would not only bring significant benefit to inform governments on the efficient use of funds across systems, but would also “inform clinicians and other service providers [across systems] on the effectiveness and appropriateness of intervention,”[2] and referral options across systems, and “consumers on the choice of service providers and treatment options.”[3]
Common issues with existing AOD data sources
Current data sources do not provide enough information to ensure system responses to people who use alcohol and other drugs is multi-dimensional and “distinguishes between occasional substance use, problematic substance use and dependence so that treatment intensity is matched to need.”[4]
One of the most common issues with the existing data sets is that the sample used to inform findings is usually not representative of the population of interest. This could be due to multiple reasons such as the sample size being too small compared to the actual population or the exclusion of particular subgroups of the sample. For example, there is currently minimal information collected to identify individuals who are members of diverse communities, especially those from culturally diverse communities.[5] According to the Queensland Mental Health Commission Don’t Judge and Listen Report, the NDSHS excludes homeless people, and those who are travelling or are in institutions such as hospitals and prisons,[6] additionally, its sampling methods assume linguistic and cultural understanding between interviewers and participants. This limitation may lead to misrepresentation of actual AOD consumption.[7] Similarly, the Drug Use Monitoring in Australia (DUMA) dataset which collects information from police detainees on drug use, interviews a low number of female detainees, thus, “caution should be exercised when interpreting the results or making gender-based comparisons.”[8]
Likewise, the AODTS NMDS which provides information on publicly funded alcohol and other drug treatment services and their clients, cannot provide information on the total number of clients who access AOD treatment. Since not all treatment services contribute to the AODTS NMDS, this dataset undercounts the number of services for young people engaged in the youth justice system and it is likely to underestimate the extent to which youth justice clients access AOD treatment services.[9]
As well, reporting biases lead to misrepresentation of the ‘average’ individual being studied (i.e. PWUD). Data completeness and uniformity are important to avoid overlooking confounding factors that create some sort of distortion of the true effect that AOD use has on PWUD. For example, the Queensland Family and Child Commission (QFCC) requested information from key government departments about the Queensland Government’s Youth Justice Strategy 2019–23 and they were told that adolescent alcohol and drug services and mental health services, especially when relating to “people with a mental disorder and a history of criminal offending,” only assess and treat clients when issues are significant, “when they may already be offending or re-offending to obtain more drugs or because of other issues in their life.”[10] The information collected in this process shall then not be used to draw conclusions about young people who use drugs and are in contact with the youth justice system, as it will over represent the severity of the issues and the effect of alcohol and other drugs. This is why it is important that datasets collect all significant information across systems, including social determinants of health to avoid perpetuating stigma.
Similarly, administrative data collected by public officers is problematic. Determining the contribution of alcohol to calls for service is constrained by “inconsistent and subjective assessments by frontline officers about the contribution of alcohol, and or poly-drug use to an incident.”[11] In the same way, reporting biases can lead to overrepresentation of particular groups in the criminal justice system such as Aboriginal and Torres Strait Islander peoples, since recording of Indigenous status in police datasets is often based on a “subjective judgement of physical appearance alone.”[12]
Data on the problematic use of alcohol among Aboriginal and Torres Strait Islander people needs to be understood within the historical and social context of colonisation, dispossession of land and culture, and social and economic disadvantage and exclusion. Factors contributing to alcohol use among Aboriginal and Torres Strait Islander people include the availability, price and marketing of alcohol, racism, and personal factors like stress, early life experiences, educational and employment disadvantage, and food insecurity. [13] (Gray, 2018)
Data consistency across jurisdictions is necessary to be able to standardise data across systems and provide a complete picture. This is why, the ongoing commitment to a cross-agency approaches is key to the success of consistent and accurate data collection that leads to complete and reliable datasets and, consequentially, leads to better-informed policy implementation.
—————————————
[1] Peter G. Miller, John Strang and Peter M., Addiction Research Methods. Blackwell Publishing Ltd, 2010.
[2] “Productivity Commission Inquiry Report on Mental Health.” Productivity Commission, 2020.
[3] Ibid.
[4] “Systemic Responses Position Paper.” QNADA, 2021.
[5]Christine Fleming, Robyn Bond, Samantha Holder and Chris Jeffries, “Evaluation of the Specialist Domestic and Family Violence Court Trial in Southport.” 15: Griffith University, 2017.
[6] “Don’t Judge and Listen: Experiences of Stigma and Discrimination Related to Problematic Alcohol and Other Drug Use.” Queensland Mental Health Commission, 2020.
[7] Ibid.
[8] “Drug and Specialist Court Review: Final Report.” Queensland Courts, 2016.
[9] “Overlap between Youth Justice Supervision and Alcohol and Other Drug Treatment Services.” Australian Institute of Health and Welfare, 2018.
[10] “Changing the Sentence: Overseeing Queensland’s Youth Justice Reforms.” Queensland Family & Child Commission, 2021.
[11] “Inquiry into Alcohol-Related Violence- Final Report.” Legislative Assembly of Queensland, Law, Justice and Safety Committee, 2010.
[12] Jacqueline Joudo, “Responding to Substance Abuse and Offending in Indigenous Communities: Review of Diversion Programs.” In Research and Public Policy Series: Australian Institute of Criminology, 2008.
[13] Dennis Gray, Kimberly Cartwright, Anna Stearne, Sherry Saggers, Edward Wilkes and Mandy Wilson, “Review of the Harmful Use of Alcohol among Aboriginal and Torres Strait Islander People.” Australian Indigenous Health Bulletin 18 (2018).
Increasing access to clinical/practice supervision among AOD workers
Courtney O’Donnell
With support from Brisbane North PHN, we are continuing our work to address the need for increased access to effective clinical/practice supervision among AOD workers in Queensland. QNADA’s Sector and Workforce Development Officer, Courtney O’Donnell, is undertaking this work as part of her PhD study at the University of Queensland (UQ) under the supervision of Professor Leanne Hides (UQ), Professor Nicole Lee (National Drug Research Institute) and Sean Popovich (QNADA).
The first phase of this project took the form of a qualitative study, which aimed to identify barriers and facilitators to accessing high quality clinical/practice supervision. Twenty-one qualitative interviews were conducted with frontline workers and service managers from eight government and non-government AOD treatment services across Brisbane. Thematic analysis indicated that there is a perceived need for all AOD workers to receive regular and frequent clinical/practice supervision from AOD specialists. Consistent with previous research, clinical/practice supervision was also perceived to have a variety of benefits for workers, their employing organisations and people who access services. Frontline workers and managers felt that barriers and facilitators to accessing effective clinical/practice supervision included limited time, the high cost of providers, availability of skilled clinical/practice supervisors, supervisor-supervisee matching and supervision modality (ie external, internal, group or individual).
During interviews, participants were also asked about their perceptions of a clinical/practice supervision exchange model. This model was developed by QNADA with the aim to increase access to effective clinical/practice supervision among workers using the limited sector resources available. A key feature of this model is that it operates on an exchange basis, whereby a worker from one organisation provides clinical/practice supervision to staff of another organisation, and vice versa. While the idea of a supervision exchange partnership was previously been suggested as a possible solution to the issue of under-resourcing in the sector, an AOD-specific clinical/practice supervision exchange model has not previously been implemented and evaluated.
Interviews revealed that frontline workers and service managers considered implementation of a clinical/practice supervision exchange model to be a resource-effective strategy to increase access to external, individual clinical/practice supervision while also exposing workers to a greater diversity of perspectives, increasing sector collaboration and improving the perceived value of clinical/practice supervision among the workforce. Participants considered potential barriers and facilitators to implementation to include willingness among services to participate, sustainability of the model and flexibility in clinical/practice supervision delivery. Data obtained from these interviews were used to inform the second phase of the study.
The second phase of this project was implementation and evaluation of a clinical/practice supervision exchange model with six participating AOD treatment services in Queensland. In late 2020, twenty frontline AOD workers (supervisees) were randomly allocated to the supervision exchange (n=10) or supervision-as-usual (n=10) arms of the study. Participants in the supervision exchange arm of the study were matched with a supervisor (n=5) employed by another participating treatment service. Supervisors and supervisees were pragmatically matched based on characteristics including years of experience in the sector, age, qualifications, expertise and interests. Monthly supervision for participants in the supervision exchange arm of the study commenced in December 2020. All participants were asked to complete a survey at baseline (0 months; pre-), 5 months (mid-supervision exchange), 10 months (post-supervision) and 15 months (follow-up). Participants were recently asked to complete the final survey and results from this trial will be available shortly.
The third phase of this project aims to identify opportunities at the service system level to increase access to effective clinical/practice supervision among the AOD workforce. As part of this project, a review of guidance documents that inform and facilitate the commissioning of AOD treatment services in Queensland is currently underway. The purpose of the review is to determine whether, and in what capacity, commissioners of services are guided to support workforce development activities, such as clinical/practice supervision, through service funding mechanisms. In addition to the review, a series of qualitative interviews with commissioners of Queensland AOD treatment services and other relevant stakeholders are being conducted. The purpose of these interviews is to: identify the perceived role and scope of commissioners of services to support the provision of clinical supervision among the AOD workforce; understand how commissioners currently support the provision of clinical/practice supervision; and identify opportunities for policymakers and commissioners of services to increase access to effective clinical/practice supervision among the workforce. Together, the review of guidelines and interviews will allow us to identify potential systemic barriers to supporting increased access to effective clinical/practice supervision, and potential opportunities to address them.
You can read the full phase one study in the journal, Drug and Alcohol Review, here – https://onlinelibrary.wiley.com/doi/full/10.1111/dar.13450
Workforce and training: The importance of cross sectoral knowledge and skills for better client outcomes
Rebecca Wen
The rapid review undertaken as part of QNADA’s Responsive Systems project examined fifty Queensland inquiries, reports and strategies undertaken in the past ten years and identified 444 recommendations and actions that are relevant to addressing alcohol and other drug related (AOD) issues across a range of systems. The findings from this review brings a valuable perspective in how cross sectoral collaboration and coordination can provide better systemic responses to improve the health and social wellbeing of individuals, families and communities that are affected by problematic AOD use.
In this article, I’ll focus on the recommendations that are related to workforce and training. There are 73 of them and it is the second largest area of focus following pathways and programs. The majority of them focuses on service improvements (27%). This includes capacity building activities for the workforce in systems such as child safety, primary health care, correction and emergency services to increase their knowledge and improve their skills about AOD related issues. For instance, Queensland Health’s Insight service has developed an AOD Brief Intervention Toolkit to help GPs and other health professionals to screen, assess and conduct brief interventions with their clients if there are concerns with AOD use. In addition, there have also been capacity building activities for our own AOD specialist workforce. Family Drug Support (FDS), for example, has expanded their service delivery scope to Central Queensland to provide workshops and information sessions for AOD and other health professionals on how to support family members who are affected by problematic AOD use.
A portion of the recommendations under service improvements is also about developing frameworks and educational recourses to encourage the communication of cross sectoral practice and knowledge. For examples, ATODA’s Domestic and Family Violence (DFV) Tools for AOD Settings provide some very practical guidance to the AOD sector on how to prevent and respond to DFV, and the recently released DFV Common risk and safety framework also includes some considerations on assessing and responding to problematic AOD use in DFV settings. A small number of the recommendations is also related to increase human resources to promote cross sectoral collaboration, such as employing youth AOD liaison staff to assist with child safety officers in some situations.
However, there are a number of recommendations that considered AOD use as a risk factor (15%) that need to be mitigated. Almost all of them are concerned about individuals displaying violent behaviours under the influence of alcohol and/or other drug. Subsequently, some workforce building and training activities were implemented, including an increase of police officers in night time precincts and the roll-out of self-defence and aggressive behaviour management trainings for ambulance and hospital staff. While these recommendations can be considered as reasonable based on the findings from their corresponding inquiries, we are apprehensive about some of the language that is used to provoke fear and marginalisation to perpetuate stigma and discrimination on people who use AOD. For example, the 2010 Inquiry into Alcohol Related Violence which has a number of recommendations related to mitigating people’s AOD use as a risk factor states:
“The Committee agrees that the majority of law abiding citizens should not have to suffer for the actions of a few……The report calls for greater enforcement and increased penalties.”
Pleasingly though, the rapid review identified a number of recommendations that are also promoting stigma reduction work (8%) across workforces. Most of these recommendations come from QMHC’s Changing attitudes, changing lives report that was released in 2018, and one strategy that has already been endorsed by the Queensland Government is the incorporation of AIVL’s ‘Putting Together the Puzzle’ anti-stigma awareness training “into existing agency training programs and professional development strategies…, for all social service sector workforces, including, health, housing, child safety and justice”[1]. The report[2] also recommended that anti-stigma trainings should be delivered in partnership with people with lived experiences of problematic AOD use as it may help to promote social inclusion and address biases and stereotypes. Some recommendations also expressed support for similar anti-stigma awareness training to be delivered to frontline police officers.
After all, it is evident from the review’s findings that, there has been efforts from a number of systems and across different workforces in Queensland attempting to address AOD related issues, and improving the wellbeing of people and communities who are affected by problematic AOD use. Most of the recommendations that focus on workforce and training have acknowledged the importance of communicating cross sectoral knowledge and building workforce capacity to provide adequate health and social care for individuals, such as responding to DFV issues in AOD settings and vice versa. Besides, I think the involvement of the AOD sector (eg the peer workforce) to provide education and trainings to other agencies about stigma reduction is in itself an effective way to reduce prejudice that some may have towards people who use alcohol and other drugs.
QNADA’s position has always been seeing the ‘person’ first while their AOD use is just one element of their life. I think this is also a belief commonly held by our members, that when a client walks through the door, they may be experiencing other difficulties in life along with their AOD use. So if QNADA can lead this momentum in facilitating better collaboration and partnership between the AOD sector and the other systems such as the child protection, youth justice, and criminal justice systems, we hope to achieve effective systemic responses to support our members to provide high quality, person centred, and evidence informed care to their clients.
————————————————————————
1Queensland Mental Health Commission, 2018. Changing attitudes, changing lives. [online] Brisbane: Queensland Mental Health Commission. Available at: https://www.qmhc.qld.gov.au/documents/changingattitudeschanginglives
2 ibid
2020-2021 Alcohol and other Drug Treatment Services National Minimum Data Set
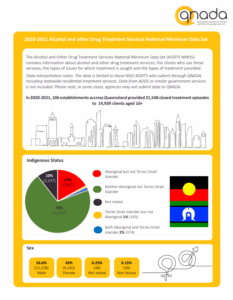
The Alcohol and Other Drug Treatment Services National Minimum Data Set (AODTS NMDS) contains information about alcohol and other drug treatment services; the clients who use these services; the type of issues for which treatment is sought and the types of treatment provided. In 2020-2021, 106 NGO AODTS establishments across Queensland submitted data to the AODTS NMDS through QNADA, including statewide residential treatment services.
The 2020-2021 submission included 21,548 closed treatment episodes to 14,939 clients aged 10+, a small increase from 21,453 episodes in 2019-20. Service responses to COVID-19 impacted treatment delivery setting in 2020. This collection year, ‘other’ delivery setting usually referred to a phone setting.
Counselling was the most accessed treatment type (50%) followed by rehabilitation (16%), and support and case management (15%). More than half of episodes were provided to male clients (57%) and around three-fourths of clients were aged 25 and over. Amphetamines remains the most common principal drug of concern for which clients sought treatment (37%), followed by Alcohols (35%) and Cannabinoids (19%).
Please click here to read the full report.
Improving pathways and programs to reduce alcohol and other drugs related harms
Courtney O’Donnell
The rapid review undertaken as part of QNADA’s Responsive Systems project sought to consider the broader system responses to individuals, families and communities affected by AOD, outside of the treatment and harm reduction sector. Specifically, it examined the ways in which the criminal justice, youth justice and child protection systems intersect with the AOD sector and respond to the social, cultural, and structural determinants of health. In total, the review identified 449 recommendations made between 2010 and 2020 which directly related to individuals, families and communities affected by AOD. Among these, more than a third (35%) focused on improving pathways and programs affecting people who use AOD.
Among the recommendations that fell within the domain of pathways and programs, a large proportion were related to enhancing treatment for people experiencing problems with their AOD use. For example, recommendations included increasing accessibility of treatment, increasing the variety of treatment types available, investing further in treatment, evaluating various existing treatment models and establishing new ones. As we know, the AOD treatment sector is chronically underfunded and overstretched, so it’s encouraging to see that a need for investment in AOD treatment has been recognised across systems. The majority of recommendations that were focused on improving treatment came from the criminal justice system, which might be expected given the high proportion of people who are in contact with the criminal justice system who also experience problems with their AOD use. At QNADA, we believe that greater availability of, and access to, AOD treatment services is crucial to ensuring that people can utilise the right services, at the right time, and in the right place.
This rapid review also illustrated that enhancing AOD treatment opportunities isn’t the only way to improve health and social outcomes for people who are engaged with the criminal justice, youth justice and child safety systems. For example, we also know that a lot of people are in contact with these systems because of their AOD use (e.g. due to criminalisation of minor drug offences). Perhaps unsurprisingly, many of the recommendations that fell within the domain of pathways and programs were centred on diversion and drug courts. Specifically, the recommendations focused on increasing access to, and tailoring, diversion and drug courts to better meet the needs of people who use drugs. This is consistent with QNADA’s position; increase police diversions and non-court support options to keep people, particularly children, out of court.
Importantly, another significant proportion of the 155 recommendations that fell within the domain of pathways and programs were focused on addressing the social determinants of health. The social determinants of health are the non-medical factors that influence health outcomes [1]. They are the conditions in which people are born, grow, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life. These forces and systems include economic policies and systems, development agendas, social norms, social policies and political systems. Identifying and addressing the social determinants that are likely to see people become engaged in the criminal justice, youth justice and child safety systems is essential to reducing engagement with those systems and problematic drug use. The majority of recommendations that were focused on addressing the social determinants of health came from the child safety system, and included: implementing initiatives to support young people living in social housing who are at risk of losing their tenancies; continuing to fund positive parenting programs; developing and expanding education, training and employment initiatives targeting young people experiencing vulnerability; and expanding initiatives to assist more young people of compulsory school age to engage in education. Implementation of recommendations of this nature, that provide support early-on to people who are vulnerable to developing problems with their AOD use, are likely to see a reduction in rates of engagement with the criminal justice, youth justice and child safety systems. These types of strategies also reduce the demand for AOD treatment and relieve pressure from the entire health system.
While there are significant reforms currently being implemented across Queensland, this review suggests there is further room for system reform. Of the 155 recommendations which fell within the domain of improving pathways and programs to reduce AOD-related harms, 23% were accepted in full, 1% were accepted in part, 2% were accepted in principle and 4.5% were not accepted. For 62% of recommendations, acceptance status could not be determined or was not applicable. Among those accepted in full, just over half (51%) were subsequently also implemented in full. Together, these findings suggest a need for increased transparency with regard to acceptance and implementation of recommendations, as well as improved processes around consultation and development of recommendations. This will likely result in greater implementation of evidence-based interventions and strategies to improve health and social outcomes.
———————–
[1] Health, C. o. S. D. o. (2008). Closing the gap in a generation: health equity through action on the social determinants of health: final report of the commission on social determinants of health: World Health Organization.
We need a better ‘addictionary’: Language and Stigma in AOD Policy and Practice
Tom Ogwang
Stigma is a complex social phenomenon. Put simply, it could be defined as “an attribute that discredits an individual in the eyes of society and results in the person being devalued, discriminated against, and labelled as deviant” [1]. Expanding on that, for stigma to take shape several interrelated elements must come together. In the first element, people must identify some social difference, and categorise it with a label accordingly. This labelling is critical, as language plays a major role in shaping people’s thoughts and beliefs[2]. The social categories identified may include people who use drugs and people who don’t, immigrants and citizens, LGBTIQ+ and heteronormative cultures, people of colour and white people, and so on[3].
In the second element, the categorizing labels are linked to dominant beliefs about the difference – stereotypes. In the third element, the stereotypes provide enough distinct social categories that they distinguish ‘us’ and ‘them’ as oppositional social identities. The above examples are commonly stereotyped into oppositional identities such as ‘criminals’ vs ‘good citizens’ or ‘deviant’ vs ‘normal’ people. The fourth element sees the stigmatised people experience status loss and discrimination that lead to unequal outcomes across every conceivable measure[4].
Discrimination is the lived experience of stigma – the negative social and material outcomes that arise from stigma, which includes lower quality of health care. Both stigma and discrimination rely on societal structures and systems that facilitate and create the conditions for their operation (for example, unequal power relations is one such condition)[5]. For these reasons stigma is harmful, distressing, and marginalising to the individuals and groups who experience it, whether based on fear and exclusion, authoritarianism, or even benevolent intentions[6].
The massive body of evidence on implicit bias and discrimination across stigmatized populations means examples of the harm of stigma abound. Research from Stanford University that systematically analysed police body camera footage of routine traffic stops shows white residents were 57 percent more likely than black residents to hear a police officer say the most respectful utterances, such as apologies and expressions of gratitude like “thank you.” Meanwhile, black community members were 61 percent more likely to hear officers say the least respectful utterances, such as informal titles like “dude” and “bro” and commands like “hands on the wheel”[7]. The study authors argued that these pervasive racial disparities in officers’ language use at best erode police-community relations. At worst they express and validate negative attitudes society holds toward people of colour, which those communities experience as institutionalised racism and deaths in custody. Such research makes it harder to trivialise or dismiss the language debate as mere “semantics” or “political correctness”, as similarly strong research abounds across all stigmatised groups, including drug using communities.
It is imperative the AOD policy, practice and research communities continue to build their understanding of how language influences the way individuals think about themselves and their ability to change, how it frames what society thinks about substance use and recovery[8] and how it influences institutional responses to substance use[9]. At the individual level, there is ample evidence the words we use to describe alcohol and other drug dependence can engender self-stigma, which occurs when a member of a target group internalises public stereotypes or prejudices[10]. This influences both whether people will seek help, and the quality of the help they receive. For instance, one study demonstrated those with alcohol use disorder perceiving a high degree of public stigma toward their condition were about half as likely to seek help as those perceiving low stigma[11]. For treating clinicians, words strongly influence the way they seek to work with people experiencing alcohol and other drug use disorders: in one Harvard study, when the term ‘substance abuser’ was used in a case vignette, clinicians were significantly more likely to favor punishment (a jail term) than when the individual was described in the vignette as having a ‘substance use disorder’[12]. It’s a short journey from the implicit bias found in that research to overt negative attitudes or discriminatory behaviours enacted by individuals acting on behalf of health or criminal justice institutions[13].
Structural stigma includes poorly chosen language, policies and actions that limit – whether intentionally or not – the opportunities of target groups. Labelling people involved in the criminal justice system – many of whose most serious offence relates to illicit drugs – ‘offenders’ for the entirety of their engagement with the criminal justice system, regardless of whether they have ceased all unlawful activity, is an overt example. Thesaurus alternatives to ‘offenders’ are ‘criminals, crooks, lawbreakers, wrongdoers, reprobates and delinquents’, all of which is language that squarely returns the individual back to the place and time of their offence, without hope of moving from there in any figurative sense until all engagement with the justice system is complete. The evidence of stigma we see across the brief examples demonstrated here, and which is experienced by all marginalised persons, is a violation of the human rights and dignity expressed in Article 1 of the Universal Declaration of Human Rights – All human beings are born free and equal in dignity and rights[14].
The QNADA rapid review of Queensland inquiries, reports and strategies relevant to the alcohol and other drug sector found evidence of stigma that powerfully shapes how the state addresses AOD use across a range of sectors[15]. It argues what is evident in many inquiries, reports and strategies is a morally bound perceptual distinction between alcohol and other drugs that defines one as being culturally acceptable and the other as immoral, illegal and deviant[16]. This returns us to the elements described above that result in stereotyped, oppositional categories, and that have been significant in how AOD policy and practice has manifested: for example, while high profile and at times experimental change in night time entertainment precinct management has been undertaken in an attempt to reduce alcohol related harm over the last ten years, responses to illicit drug use have remained largely unchanged during the same period. Far more than just words, at the institutional level language ‘influences recommendation acceptance, shapes the approach taken to implementation, program design and workforce development, and is used to inform future policy and legislative priorities’[17].
There is a lot of work to be done in the stigma and discrimination space. It isn’t overly complex though, and perhaps begins with the universal use of person-centred (or person-first) language to describe groups at the margins of society[18]. This is especially true of people who use drugs and who are also, for example, at the intersections of minority ethnicities, genders or sexualities. Given outstanding materials like this Language matters resource, not only does the AOD sector have its own waypoints, but it is well equipped to begin charting this journey outside its own boundaries and in such spaces as the media and other public discourses where the public gets most of its information about alcohol and other drug use.
—————————————
[1] Lancaster, K., Seear, K., Ritter, A. (2017) Reducing Stigma and Discrimination for People Experiencing Problematic Alcohol and Other Drug Use (Queensland Mental Health Commission).
[2] Volkow, N.D., Gordon, J.A., Koob, G.F. (2021) Choosing appropriate language to reduce the stigma around mental illness and substance use disorders. Neuropsychopharmacology. July 2021
[3] Link, B. G., & Phelan, J. C. (2001). Conceptualizing Stigma. Annual Review of Sociology, 27, 363-385.
[4] Ibid
[5] Lancaster, K., Seear, K., Ritter, A. (2017) Reducing Stigma and Discrimination for People Experiencing Problematic Alcohol and Other Drug Use (Queensland Mental Health Commission).
[6] Broyles,L.M., Binswanger, I.A., et al (2014) Confronting Inadvertent Stigma and Pejorative Language in Addiction Scholarship: A Recognition and Response. Substance Abuse 35:217-221
[7] Voigt, R., Camp, N.P., et al (2017) Language from police body camera footage shows racial disparities in officer respect. Proceedings of the Natural Academy of Sciences of the United States of America
[8] Broyles,L.M., Binswanger, I.A., et al (2014) Confronting Inadvertent Stigma and Pejorative Language in Addiction Scholarship: A Recognition and Response. Substance Abuse 35:217-221
[9] Wogen, J. and Restrepo M.T. (2020) Human rights, stigma, and substance use. Health and Human Rights 22(1):51-60
[10] Ibid
[11] Keyes K.M., Hatzenbuehler M.L., McLaughlin K.A., Link B., Olfson M., Grant B.F., (2010) Stigma and treatment for alcohol disorders in the United States. American Journal of Epidemiology; 172:1364–72. .
[12] Kelly J.F., Westerhoff C.M. (2010) Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. International Journal of Drug Policy 21:202–7
[13] Wogen, J. and Restrepo M.T. (2020) Human rights, stigma, and substance use. Health and Human Rights 22(1):51-60
[14] United Nations (1948) Universal Declaration of Human Rights. www.un.org/en/about-us/universal-declaration-of-human-rights
[15] QNADA (2021) Responsive Systems: A rapid review of Queensland inquiries, reports and strategies relevant to the alcohol and other drug sector.
[16] QNADA (2021) Responsive Systems: A rapid review of Queensland inquiries, reports and strategies relevant to the alcohol and other drug sector.
[17] Ibid
[18] Lancaster, K., Seear, K., Ritter, A. (2017) Reducing Stigma and Discrimination for People Experiencing Problematic Alcohol and Other Drug Use (Queensland Mental Health Commission).